Expert Intervention in Oral Health: What Is Oral, Dental, and Maxillofacial Surgery?
Oral, dental, and maxillofacial surgery is a specialized branch of dentistry that involves the surgical treatment of teeth, jawbones, and soft tissues within the mouth. It includes a wide range of procedures such as impacted tooth extraction, cyst or tumor removal, jaw fracture treatment, and implant surgery. Especially in cases that require precision and expertise, procedures performed by experienced surgeons in this field play a vital role in maintaining oral and jaw health.
When Is It Applied?
-
Extraction of impacted wisdom teeth
-
Cyst and tumor removal operations
-
Jaw fractures and temporomandibular joint (TMJ) disorders
-
Dental implant placement
-
Abscess drainage and infection treatment
-
Bone grafting after tooth extraction
-
Sinus lifting (sinus floor elevation)
Advantages of Oral, Dental, and Maxillofacial Surgery
-
Safe removal of diseased tissues
-
Preparation of oral structure for prosthetic or implant treatments
-
Long-term and integrated treatment solutions
-
Elimination of pain, swelling, and infection-related issues
-
Faster healing with accurate and minimally invasive interventions
Treatment Process and Application
The process begins with a detailed intraoral and radiological examination. In some cases, 3D tomography is used to evaluate the jaw structure. Surgical procedures are performed under local anesthesia and, if necessary, with sedation or general anesthesia. Post-operative recovery time varies depending on the patient and the complexity of the procedure.
Frequently Asked Questions
-
Is impacted tooth extraction painful?
No. The procedure is performed under local anesthesia, so no pain is felt. Mild swelling or discomfort afterward can be managed with prescribed medication.
-
How long does it take to recover after jaw surgery?
Typically, recovery occurs within a week, although larger operations may require more time.
-
Can I eat after the surgery?
Soft and liquid foods are recommended for the first 24 hours. Avoid hot food, beverages, and smoking.
-
Can every dentist perform jaw surgery?
No. This field requires specialized training and experience. For complex cases, patients should consult an oral and maxillofacial surgeon.
-
Will my face swell after the surgery?
Temporary swelling may occur after some surgical procedures. Applying ice helps reduce swelling effectively.

The Last Resort in Dental Health: What Is Tooth Extraction?
Tooth extraction is the process of removing a tooth from the mouth, either surgically or simply, when it can no longer remain healthy due to decay, trauma, infection, or lack of space. Although modern dentistry prioritizes preserving the natural tooth, extraction becomes inevitable in some cases.
When performed correctly and under sterile conditions, tooth extraction is a safe and quick procedure that protects the patient’s overall health and prepares the mouth for future treatments.
When Should a Tooth Be Extracted?
Advanced tooth decay that cannot be treated
Fractured or cracked teeth (especially below the gum line)
Teeth loosened by gum disease and bone loss
Extractions for orthodontic preparation
Impacted or partially erupted wisdom teeth
Cysts, abscesses, or infections at the root area
Irreversible trauma to the tooth
How Is Tooth Extraction Performed?
There are two main types of extraction:
Simple Extraction:
Used for visible teeth that are easy to access. Performed under local anesthesia, the tooth is loosened and removed with special instruments.
Surgical Extraction:
Used for impacted or broken teeth. The gum is opened and, if necessary, some bone tissue is removed. The area is cleaned and sutured afterward.
Both methods are painless during the procedure, and with proper aftercare, recovery is usually smooth.
Post-Extraction Care Instructions
Do not rinse or spit for 24 hours
Avoid eating or drinking for the first 2 hours
Stay away from hot food and beverages for 24 hours
Do not smoke or consume alcohol
Apply pressure with a gauze pad for 30 minutes
Use cold compresses to reduce swelling
Maintain oral hygiene but avoid brushing the extraction site aggressively
Take antibiotics or painkillers if prescribed
What Happens After a Tooth Is Extracted?
If the missing tooth is not replaced, the neighboring teeth may shift toward the empty space, leading to:
Crooked teeth
Chewing difficulties
Aesthetic issues
Jaw joint imbalance
Bite misalignment
Therefore, options such as implants, bridges, or dentures should be considered after extraction.
Frequently Asked Questions
Does tooth extraction hurt?
No. Local anesthesia prevents pain during the procedure. Mild discomfort afterward can be managed with medication.
How long does bleeding last?
Minor oozing may continue for a few hours. If bleeding persists beyond 24 hours, contact your dentist.
Can I smoke after extraction?
No. Smoking delays healing and increases the risk of “dry socket” infection.
When are stitches removed?
Typically after 7–10 days. Dissolvable stitches may not require removal.
When can I eat again?
Avoid eating for 2 hours, then consume only soft, lukewarm foods for the first 24 hours.

Say Goodbye to Impacted and Problematic Teeth: What Is a Wisdom Tooth?
Wisdom teeth (third molars) usually emerge between the ages of 17 and 25 and are located at the very back of the mouth. In many cases, due to limited jaw space, these teeth cannot erupt properly and remain partially or fully impacted. Impacted wisdom teeth can cause pain, swelling, infection, tooth decay, and even jaw misalignment.
For this reason, wisdom tooth extraction often becomes an inevitable step in maintaining oral health.
When Should a Wisdom Tooth Be Extracted?
Fully impacted: The tooth is completely trapped within the gum or bone.
Partially impacted: Part of the tooth has erupted while the rest remains covered by gum tissue, increasing infection risk.
Decayed or infected: Wisdom teeth are hard to clean and easily decay.
Causing pressure on adjacent teeth: Can lead to crowding or misalignment.
Cyst formation: Cysts or bone loss may develop around impacted teeth.
Before orthodontic treatment: To prevent shifting of other teeth.
How Is a Wisdom Tooth Extracted?
The procedure depends on the tooth’s position:
Simple Extraction:
If the tooth is fully erupted and accessible, it can be removed quickly under local anesthesia.
Surgical Extraction:
If the tooth is embedded in the gum or bone, a small incision is made in the gum. Sometimes a small amount of bone is removed, and the tooth is sectioned for easier extraction. Stitches are then placed, and healing begins within a few days.
How Long Does the Procedure Take?
Simple extractions take about 10–15 minutes, while surgical extractions may take 30–45 minutes, depending on the tooth’s position and the individual’s anatomy.
Post-Extraction Care
Avoid hot foods and drinks for 24 hours.
Do not rinse or spit for the first day.
Avoid smoking and alcohol for at least 2 days.
Apply a cold compress to reduce swelling.
Take antibiotics and painkillers as prescribed.
Avoid hard, grainy, or spicy foods.
Stitches are usually removed after 7–10 days.
Possible Complications
Swelling and pain: Common for the first 2–3 days.
Dry socket (alveolitis): Occurs when the blood clot dislodges, causing infection and pain.
Jaw stiffness or muscle spasm: May occur, especially with lower wisdom teeth.
Numbness: Temporary numbness can occur if nerves are close to the tooth root.
These effects are typically temporary and manageable with proper care.
Frequently Asked Questions
Is wisdom tooth extraction painful?
No. It is performed under local anesthesia, so no pain is felt during the procedure. Mild pain afterward can be managed with medication.
Do all wisdom teeth need to be extracted?
No. If they erupt properly, can be cleaned, and don’t harm surrounding tissues, extraction is unnecessary.
Are lower wisdom teeth harder to remove?
Yes. The lower jawbone is denser, making surgical extraction slightly longer and more delicate.
Can wisdom teeth cause misalignment?
Yes. Impacted or angled wisdom teeth can push other teeth forward, causing crowding, especially in the front.
How long does healing take?
Initial healing occurs within 3 days, and complete recovery takes about 7–10 days. Your dentist will determine if and when stitches need to be removed.
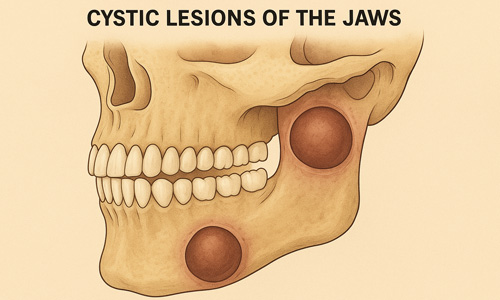
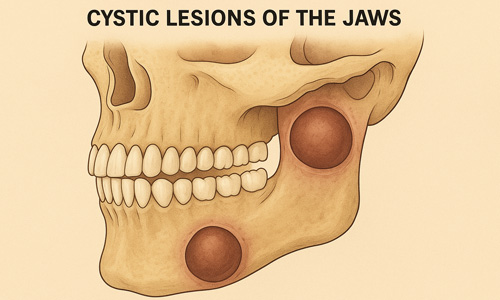
The Silent Danger Inside the Mouth: Dental and Jaw Cysts
Cysts that form in the mouth, teeth, or jaw region are often asymptomatic at first but can gradually damage surrounding tissues as they grow. These cysts may develop around tooth roots, within the jawbone, or in soft tissues, leading to tooth loss, bone resorption, infections, or even jaw fractures if left untreated.
Cyst removal surgery involves the surgical cleaning and elimination of these harmful formations to protect oral health. With early diagnosis and proper treatment, patients can regain both a healthy and aesthetically balanced oral structure.
Common Types of Oral and Jaw Cysts
Radicular Cyst: The most common type, typically developing around the roots of decayed or dead teeth.
Dentigerous (Follicular) Cyst: Forms around unerupted (impacted) teeth.
Periodontal Cyst: Occurs in association with gum tissue.
Residual Cyst: Develops in the area where a tooth was previously extracted.
Keratocystic Cyst: A more aggressive type with a high recurrence risk.
Symptoms of Jaw and Dental Cysts
While many cysts are discovered incidentally during routine X-rays, advanced cases can show symptoms such as:
Swelling in the tooth or jaw area
Hardness or palpable lump
Oral pain or sensitivity
Tooth displacement or loosening
Abscess or discharge formation
Facial asymmetry or swelling
Thinning of the jawbone
How Is Cyst Removal Surgery Performed?
Treatment depends on the cyst’s type, size, and location:
Small Cysts:
Infected tissue is cleaned under local anesthesia, and the area is sterilized. The associated tooth may also be extracted if necessary.
Large Cysts:
A surgical incision is made, and the entire cyst wall is removed. Bone grafts may be applied to restore the jaw structure. The area is then sutured.
Cysts Around Impacted Teeth:
The cyst is removed together with the impacted tooth. These cases usually require longer surgery and recovery periods.
Post-Operative Care
Take prescribed antibiotics and painkillers as directed.
Apply cold compresses within the first 24 hours to reduce swelling.
Avoid hot, hard, or irritating foods for 48 hours.
Refrain from smoking and alcohol consumption.
Maintain oral hygiene gently—do not brush the surgical site vigorously.
Stitches are usually removed after 7–10 days.
Attend all follow-up appointments as scheduled.
If Left Untreated, Cysts Can Cause:
Bone resorption in the jaw
Tooth displacement or loss
Nerve damage and numbness
Facial deformities
Recurrent infections
Rarely, transformation into a tumor
Frequently Asked Questions
Is cyst removal surgery painful?
No. It is performed under local anesthesia, so no pain is felt during the procedure. Mild pain or swelling afterward can be managed with medication.
Can cysts recur?
Yes, some types (such as keratocystic cysts) have a tendency to recur. Regular follow-ups are essential.
How long does recovery take?
Initial healing typically begins within 7–10 days, but larger cysts may require a longer recovery period.
Does bone regenerate after cyst removal?
Yes. In most cases, bone gradually regenerates, though bone grafting may be necessary for larger cavities.
Are all cysts surgically removed?
No. Small, inactive cysts may be monitored, but enlarging or infected cysts require surgical removal.
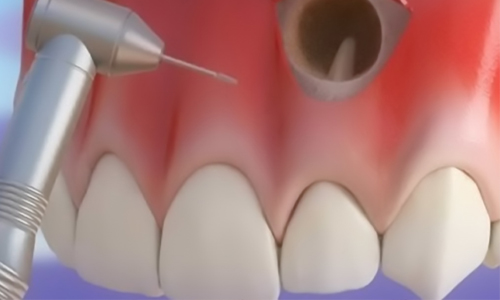
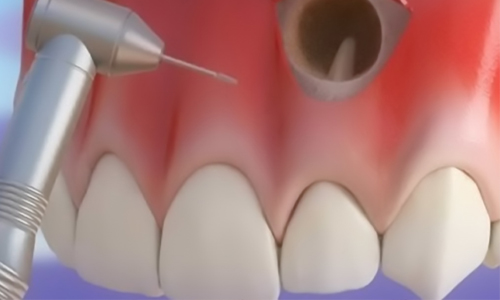
Surgical Solution for Root-End Infections
Apical resection is a surgical procedure performed to remove infected tissue at the tip of a tooth root when a root canal treatment has failed to heal or has become re-infected. It is generally applied in cases where pain, abscess, or cystic formations are seen radiologically after root canal therapy. This operation is one of the final steps to save the tooth without extraction.
The infected tissue at the root tip, and sometimes a small portion of the root itself, is removed. During the procedure, the end of the root canal is sealed with special materials to prevent reinfection.
When Is Apical Resection Performed?
When an infection persists despite root canal treatment
When a cyst or granuloma develops at the root tip
In cases of persistent pain and swelling around the tooth
When a second root canal treatment is not possible
When repeating root canal treatment is risky or ineffective
When the root tip is curved or fractured, making conventional treatment unsuccessful
How Is Apical Resection Performed?
The area is numbed with local anesthesia.
The gum is opened and the jawbone is gently removed to access the root tip.
The infected tissue and part of the root are excised.
The root canal tip is disinfected and sealed with a leak-proof filling material.
The area is cleaned, stitched, and the procedure is completed.
Antibiotics and painkillers may be prescribed if necessary.
The procedure typically takes 30–45 minutes, and thanks to local anesthesia, the patient feels no pain.
Advantages of Apical Resection
Treats persistent infections without tooth extraction
Helps preserve the natural tooth
Provides fast and effective results
With successful application, the tooth can last for many years
Completely eliminates cysts and granulomas
Post-Treatment Care
Avoid hot food and drinks for the first 24 hours
Apply an ice compress to prevent swelling (for the first 6–8 hours)
Brush gently, avoiding pressure on the treated area
Refrain from smoking or alcohol for at least 48 hours
Take prescribed antibiotics and painkillers as directed
Stitches are usually removed within 7–10 days
Do not skip follow-up appointments
What to Expect After the Procedure
Mild swelling and pain are normal
Slight tenderness may persist for a few days
Temporary numbness or bruising may rarely occur
Relief is usually felt within a week; persistent symptoms should be evaluated by the dentist
Frequently Asked Questions
Is apical resection painful?
No. It is performed under local anesthesia, so no pain is felt during the procedure. Mild pain or sensitivity may occur afterward.
Is this procedure a substitute for root canal treatment?
No. Apical resection is performed on a tooth that has already undergone root canal therapy when it fails to heal.
How long will the tooth last after the operation?
With successful treatment, the tooth can remain functional for many years.
Can all teeth undergo apical resection?
Not always. It may be difficult to apply to multi-rooted teeth in the back of the mouth. The dentist decides after examination.
Will swelling occur after the operation?
Yes, slight swelling may occur. This can be managed with ice compresses and prescribed medications.