Sitemizdeki deneyiminizi geliştirmek için çerez kullanıyoruz. Sitemizi kullanarak çerezlere izin vermiş olursunuz. Daha fazla

Oral, Dental and Maxillofacial Surgery
Expert Intervention in Oral Health: What Is Oral, Dental, and Maxillofacial Surgery?
Oral, dental, and maxillofacial surgery is a specialized branch of dentistry that involves the surgical treatment of teeth, jawbones, and soft tissues within the mouth. It includes a wide range of procedures such as impacted tooth extraction, cyst or tumor removal, jaw fracture treatment, and implant surgery. Especially in cases that require precision and expertise, procedures performed by experienced surgeons in this field play a vital role in maintaining oral and jaw health.
When Is It Applied?
Extraction of impacted wisdom teeth
Cyst and tumor removal operations
Jaw fractures and temporomandibular joint (TMJ) disorders
Dental implant placement
Abscess drainage and infection treatment
Bone grafting after tooth extraction
Sinus lifting (sinus floor elevation)
Advantages of Oral, Dental, and Maxillofacial Surgery
Safe removal of diseased tissues
Preparation of oral structure for prosthetic or implant treatments
Long-term and integrated treatment solutions
Elimination of pain, swelling, and infection-related issues
Faster healing with accurate and minimally invasive interventions
Treatment Process and Application
The process begins with a detailed intraoral and radiological examination. In some cases, 3D tomography is used to evaluate the jaw structure. Surgical procedures are performed under local anesthesia and, if necessary, with sedation or general anesthesia. Post-operative recovery time varies depending on the patient and the complexity of the procedure.
Frequently Asked Questions
Is impacted tooth extraction painful?
No. The procedure is performed under local anesthesia, so no pain is felt. Mild swelling or discomfort afterward can be managed with prescribed medication.
How long does it take to recover after jaw surgery?
Typically, recovery occurs within a week, although larger operations may require more time.
Can I eat after the surgery?
Soft and liquid foods are recommended for the first 24 hours. Avoid hot food, beverages, and smoking.
Can every dentist perform jaw surgery?
No. This field requires specialized training and experience. For complex cases, patients should consult an oral and maxillofacial surgeon.
Will my face swell after the surgery?
Temporary swelling may occur after some surgical procedures. Applying ice helps reduce swelling effectively.

Prosthetic Dental Treatments
Functional and Aesthetic Restoration of Lost Teeth
Prosthetic dental treatments are a branch of dentistry that aims to restore teeth lost or damaged due to various reasons — both functionally and aesthetically. These treatments help patients regain proper chewing ability, speech, and a natural-looking smile. Whether fixed or removable, prosthetic restorations not only support oral health but also significantly improve quality of life.
Tooth loss is not merely an aesthetic concern; it can also cause chewing difficulties, digestive problems, jaw joint disorders, and shifting of remaining teeth. Prosthetic treatments are personalized solutions designed to eliminate these negative effects.
Types of Prosthetic Dental Treatments
Fixed Prostheses (Bridges and Crowns):
Spaces caused by missing teeth are closed using porcelain, zirconium, or E-max crowns supported by adjacent healthy teeth.
Removable Prostheses (Full or Partial Dentures):
Used when the jawbone or surrounding teeth cannot support fixed restorations. These dentures can be easily inserted and removed by the patient.
Implant-Supported Prostheses:
Applied over dental implants placed in the jawbone to replace missing teeth. These can be either fixed or removable.
Temporary Prostheses:
Short-term solutions used to maintain aesthetics and function until permanent restorations are completed.
When Are Prosthetic Treatments Needed?
In cases of tooth loss
When teeth have severe structural damage
When teeth are misshapen or discolored
For completely edentulous patients (total dentures)
For patients requiring implant-supported fixed teeth
Advantages of Prosthetic Treatments
Restores chewing and speech functions
Improves self-confidence through aesthetic enhancement
Supports facial structure, preventing premature aging
Prevents misalignment of remaining teeth
Provides durable, long-lasting results
Treatment Process
During the first consultation, the patient’s oral condition, missing teeth, bone structure, and expectations are evaluated. Measurements are taken, and the prosthesis is custom-made in a dental laboratory. After one or two fitting sessions, the prosthesis is permanently placed or delivered to the patient. Adaptation usually occurs within a short time.
Frequently Asked Questions
What is the difference between fixed and removable prostheses?
Fixed prostheses are cemented and cannot be removed by the patient. Removable ones can be inserted and taken out freely.
Do prostheses look like natural teeth?
Yes. Especially with modern materials such as zirconium and E-max, fixed prostheses can achieve an appearance very close to natural teeth.
Do prostheses cause pain?
A slight discomfort may occur initially, but patients adapt quickly. Adjustments can be made if necessary.
Do removable dentures affect speech or chewing?
There may be a short adjustment period, but with regular use, speech and chewing functions return to normal.
How long do prostheses last?
With proper care and regular dental check-ups, prostheses can last 5–10 years. Over time, they may need replacement due to natural changes in oral anatomy.

Periodontology
Healthy Teeth Begin with Healthy Gums
Periodontology is the branch of dentistry that focuses on protecting the health of the soft tissues (gums) and hard tissues (alveolar bone) surrounding the teeth, as well as treating diseases that develop in these areas. Gum diseases often progress silently and, if left untreated, can eventually lead to tooth loss. Therefore, periodontology plays a vital role not only in treating symptoms like gum bleeding but also in maintaining overall oral health.
The strength of teeth depends not only on their structure but also on the health of the surrounding gum and bone tissue. For this reason, gum care is essential for long-lasting oral health and aesthetic smiles.
Types of Gum Diseases
Gingivitis:
The early stage of gum inflammation. Symptoms include gum bleeding, swelling, and tenderness. It is reversible with regular cleaning and proper oral hygiene.
Periodontitis:
An advanced form of gum disease. It involves gum recession, bone loss, and tooth mobility. Without treatment, it can result in tooth loss.
Periodontal Treatment Methods
Scaling (Tartar Cleaning): Removes plaque and tartar from the surface of the teeth.
Curettage (Deep Cleaning): Cleans inflamed tissues beneath the gumline using special instruments.
Laser Gum Treatment: Kills bacteria and accelerates healing using laser technology.
Periodontal Surgery: In advanced cases, surgical access is provided to clean infected areas and reshape the gums.
Bone Grafts and Regenerative Procedures: Used to regenerate lost bone tissue in severe cases of bone loss.
When Should You See a Periodontist?
Gum bleeding
Swollen, red, or tender gums
Gum recession
Loose or shifting teeth
Persistent bad breath
Gaps forming between teeth
Poorly fitting dentures
Treatment Process
The treatment plan depends on the severity of the disease. In mild cases such as gingivitis, professional cleaning and maintenance may be sufficient. For advanced periodontitis, surgical intervention may be required. With consistent dental care and regular check-ups, gum health can be maintained effectively.
Frequently Asked Questions
What happens if gum disease is left untreated?
The infection spreads from the gums to the bone, leading to bone loss, tooth mobility, and ultimately tooth loss.
Is gum disease contagious?
No. However, poor hygiene among family members can lead to the development of similar bacterial flora.
Is curettage painful?
No. The procedure is performed under local anesthesia, and only mild sensitivity may occur afterward.
Can gum recession be reversed?
In advanced cases, gum grafts can partially restore the lost tissue, though complete reversal is not always possible.
What causes gum disease?
Poor oral hygiene, smoking, stress, systemic conditions (such as diabetes), genetic predisposition, and improperly made fillings or prostheses can trigger gum disease.

Implantology
A Permanent and Aesthetic Solution for Tooth Loss: Dental Implants
Implantology is a branch of dentistry that offers the most natural and long-lasting solution for missing teeth by placing artificial roots (implants) into the jawbone. These titanium implants act as tooth roots, over which prosthetic crowns are fixed. This method restores both aesthetics and functionality—allowing patients to regain normal chewing, speaking, and smiling abilities.
Dental implants are suitable not only for single-tooth replacements but also for multiple missing teeth or even completely edentulous (toothless) jaws.
When Are Dental Implants Recommended?
Single or multiple tooth loss
Completely edentulous jaws (implant-supported dentures)
Patients who do not wish to use removable dentures
Individuals who prefer not to file down healthy teeth for bridgework
Those experiencing chewing or speech problems due to tooth loss
Patients seeking a natural and aesthetic smile restoration
How Is the Dental Implant Procedure Performed?
During the initial examination, the dentist evaluates the jawbone using X-rays or 3D tomography if necessary. If sufficient bone density is present, the implant is placed under local anesthesia. It typically takes 2–3 months for the implant to integrate with the bone (osseointegration). After healing, a prosthetic crown is attached to the implant. With modern technology, in suitable cases, implants can even be restored with fixed crowns on the same day.
Advantages of Dental Implants
Closest solution to natural teeth
No damage to neighboring teeth
Long-lasting and highly durable
Provides excellent aesthetic results
Prevents bone loss in the jaw
Restores chewing and speech functions
Post-Treatment Care
Avoid hot food and beverages for the first 24 hours
Do not smoke or consume alcohol, as they delay healing
Keep the implant area clean and brush as instructed by your dentist
Attend regular dental check-ups
Avoid biting on hard objects
Frequently Asked Questions
Is the implant procedure painful?
No. It is performed under local anesthesia and is generally painless. Mild sensitivity afterward can be managed with simple painkillers.
Can everyone have implants?
Yes, if the bone structure and general health are suitable. However, conditions such as diabetes or osteoporosis require special evaluation.
Do implants last a lifetime?
With proper application and regular care, implants can last 20 years or even longer.
Can the body reject the implant?
No. Titanium is 100% biocompatible with the human body, and rejection or allergic reactions are extremely rare.
How long does the treatment take?
Depending on the bone condition and technique, the treatment duration can vary from 1 day to 3 months.

Special Topics
Every Smile Has Its Story: Personalized Dental Approaches for You
In dentistry, every patient has unique needs, expectations, and oral structures. The “Special Topics” category covers personalized treatment processes designed for cases that go beyond classical dental procedures — situations requiring a multidisciplinary approach or cases that cannot be resolved with standard methods.
Sometimes, a patient’s expectations, medical condition, oral anatomy, or previous dental treatments require expertise and planning that exceed conventional dental procedures. The “special topics” approach focuses entirely on patient-specific, individualized care — offering a tailor-made treatment journey.
Which Cases Fall Under “Special Topics”?
Complex implant treatments (such as bone resorption or sinus sagging)
Combined cases involving smile design and aesthetic rehabilitation
Multimodal treatments (e.g., aligner orthodontics + veneers)
Advanced temporomandibular joint (TMJ) disorders
Bruxism (teeth grinding) and night guard applications
Digital dentistry (3D scanning, CAD/CAM-assisted restorations)
Use of metal-free materials for patients with allergies
Individuals seeking both medical and aesthetic outcomes
How Is a Personalized Treatment Plan Created?
Comprehensive Oral Examination: Radiographic evaluation and digital scans are performed.
Listening to the Patient’s Expectations: Lifestyle, medical history, and aesthetic goals are analyzed.
Multidisciplinary Assessment: Specialists collaborate (implantology, orthodontics, periodontology, etc.).
Customized Treatment Plan: Each step of the process is clearly explained and individually applied.
Advantages
Provides effective, patient-specific solutions
Allows multiple issues to be addressed in one plan
Ensures high patient satisfaction and long-term success
Supported by the latest dental technologies
Achieves both functional and aesthetic harmony
Treatment Duration and Process
Since “special topics” often involve multiple disciplines, treatment times can be longer. However, thanks to detailed pre-treatment planning, the process remains predictable. Patients are informed step by step, and each stage is personalized according to their needs.
Frequently Asked Questions
Which treatments are included under special topics?
Combined or advanced procedures such as implants, orthodontics, veneers, TMJ therapy, and digital dentistry fall under this category.
Does every patient require a special treatment plan?
No. Personalized planning is reserved for complex cases that require additional expertise or advanced technology beyond standard methods.
Does the treatment process take longer?
It depends on the case. However, because everything is pre-planned, both timing and cost are clearly communicated from the start.
Are special treatments more expensive?
Since they are comprehensive and customized, costs may vary from standard treatments. Nonetheless, all details are transparently shared with the patient beforehand.
What is digital planning?
It is an advanced technological process using 3D scanning and computer-assisted software to ensure precision, speed, and predictable results.

Pedodontics (Pediatric Dentistry)
The Foundation of Healthy Smiles Begins in Childhood
Pedodontics (Pediatric Dentistry) is the branch of dentistry dedicated to maintaining the health and development of primary and permanent teeth in children aged 0–13, as well as providing treatment when necessary. This field requires specialized approaches tailored to children’s physical and psychological needs, making it a highly sensitive and skilled area of dentistry.
Pediatric dentistry is not limited to treating cavities; it also includes dental development monitoring, trauma management, preventive applications, and orthodontic guidance. The oral hygiene habits developed during childhood are the key to a lifetime of healthy teeth and confident smiles.
Pediatric Dental Treatments Include:
Preventive Dentistry: Cavity-preventive applications such as fissure sealants and fluoride treatments
Cavity Treatments: Fillings and root canal therapy for both primary and permanent teeth
Tooth Extractions: Removal of decayed or naturally shedding teeth
Space Maintainers: Devices to preserve the space for permanent teeth after early loss of primary teeth
Trauma Management: Emergency treatment for tooth fractures or falls
Habit-Breaking Appliances: Tools to help prevent habits like thumb sucking or nail biting
Early Orthodontic Guidance: Monitoring jaw growth and tooth alignment at an early stage
Why Choose a Pedodontist?
Children’s oral structures and emotional responses differ from adults, which is why pedodontists:
Use communication and techniques suited to child psychology
Reduce fear and anxiety through friendly, patient-centered approaches
Offer a gentle and understanding treatment process
Monitor developmental changes with precision
Help children build long-term trust and comfort with dental visits
When Should Your Child Visit the Dentist?
According to the World Health Organization and the Turkish Society of Pediatric Dentistry, a child’s first dental visit should take place when the first tooth erupts, or by age one at the latest. This visit helps familiarize the child with the dental environment and establishes a positive start to lifelong oral care.
Preventing Dental Fear: Early Visits Build Confidence
Most dental fears in children stem from parents’ attitudes or painful first experiences at older ages. Early and gentle dental visits, guided by a pedodontic approach, help children form trust and comfort. Colorful fillings, playful introductions, and explanatory storytelling make the experience both fun and educational.
Frequently Asked Questions
Do baby teeth really need treatment since they will fall out anyway?
Yes. Baby teeth are essential for chewing, speech, and guiding permanent teeth. Early loss may lead to misalignment or developmental issues in the jaw.
Is fluoride treatment harmful?
No. When applied in the correct dose under professional supervision, fluoride reduces cavity formation by 40–60%.
What is a space maintainer and why is it used?
It is an appliance used to preserve the space for a permanent tooth after early loss of a baby tooth, preventing crowding or misalignment.
How can dental fear be prevented?
Introducing the dentist early with painless, positive visits helps build trust. Avoid forcing the child and allow the dentist to establish a friendly connection.
At what age should brushing habits begin?
Oral cleaning should start when the first tooth appears. From age 2, fluoride toothpaste can be used. Parental supervision is recommended until age 6–7.

Orthodontics
The Key to Straight Teeth and a Healthy Smile
Orthodontics is a branch of dentistry that corrects irregularities in the teeth and jaws, aiming to achieve both aesthetic and functional oral harmony. Problems such as crowded teeth, jaw misalignment, bite irregularities, or tooth gaps can be corrected through orthodontic treatment. This not only enhances facial aesthetics but also improves chewing and speech functions.
Today, orthodontic treatment is not limited to children and teenagers; adults can also benefit from it. Especially with clear aligners, treatment can be completed without visible braces, providing both comfort and aesthetics.
Common Orthodontic Problems
Orthodontic treatment is required for conditions such as:
Crowded or overlapping teeth
Gaps between teeth (diastema)
Upper or lower jaw protrusion or retrusion
Open bite or deep bite
Jaw misalignment between upper and lower jaws
Crossbite
Tooth misalignment caused by premature or delayed loss of baby teeth
These problems affect not only appearance but also oral health. Severe crowding can make brushing difficult, leading to cavities and gum disease.
Orthodontic Treatment Methods
Orthodontic treatments are personalized according to the patient’s needs and aesthetic preferences. The main modern methods include:
Metal Braces (Brackets)
The most common and traditional method. Modern versions are smaller and more comfortable, often preferred by young patients.
Ceramic (Aesthetic) Braces
Made of tooth-colored materials that are less visible. Ideal for patients who value appearance during treatment.
Clear Aligners (Invisible Orthodontics)
A system like Invisalign that uses removable, nearly invisible trays. They are comfortable, hygienic, and aesthetic — suitable for mild to moderate cases.
Lingual Orthodontics
Brackets are placed on the inner surface of the teeth, making them completely invisible. The technique is highly specialized and may require a longer adjustment period.
At What Age Can Orthodontic Treatment Be Done?
The ideal time for orthodontic treatment is between ages 9–14, while jaw growth is still active. However, with modern advancements, adults can also undergo orthodontic treatment safely. Age is no barrier — what matters is healthy teeth and bone structure.
Advantages of Orthodontic Treatment
Creates an aesthetic and confident smile
Improves chewing and speech
Makes oral hygiene easier
Reduces the risk of cavities and gum disease
Helps prevent jaw joint problems
Boosts self-confidence and social comfort
Treatment Process and Check-ups
Treatment duration depends on the severity of the issue and the chosen method, usually lasting between 12 and 24 months.
For clear aligner treatments:
Aligners are changed every 9–10 days.
Check-ups every 5–6 weeks are recommended.
Aligners should be worn 20–22 hours per day.
For braces, monthly visits are scheduled for wire adjustments. Maintaining good oral hygiene and attending regular appointments are key to treatment success.
Frequently Asked Questions
Is orthodontic treatment painful?
Mild pressure or soreness may occur at the beginning but usually disappears within a few days.
Can adults have orthodontic treatment?
Yes. Orthodontics is possible at any age, provided teeth and bone are healthy.
Who is suitable for clear aligner treatment?
Patients with mild to moderate misalignments. For more complex cases, traditional braces are preferred.
Do braces affect speech?
There may be a short adjustment period, but speech usually returns to normal within a few days.
Will teeth move back after treatment?
No, as long as retainers or night guards are used. These devices prevent relapse and maintain the achieved alignment.
Endodontics (Root Canal Treatment)
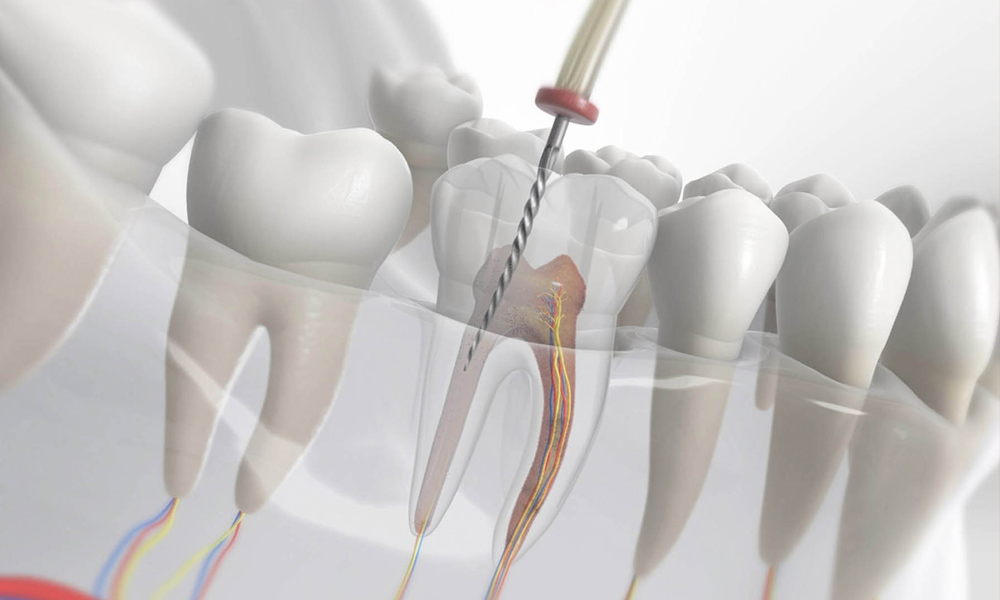
The Most Effective Way to Save a Tooth: What Is Root Canal Treatment?
Endodontics, commonly known as “root canal treatment,” is a dental procedure applied when the tooth’s inner nerve and vascular tissues become infected. Due to deep decay, trauma, or damaged old fillings, the dental pulp (nerve tissue) may become inflamed or die. During treatment, this infected tissue is removed, the canals are shaped and disinfected, and then filled with a special sealing material. As a result, the tooth can remain functional and healthy in the mouth for many years without extraction.
Root canal treatment is not merely a “last resort” to save a tooth—it is a modern, reliable, and long-term solution when performed correctly.
When Is Root Canal Treatment Needed?
When decay reaches the nerve of the tooth
Following dental trauma (fractures, cracks)
Sensitivity after deep fillings
Persistent toothache, throbbing pain, or night pain
Abscess or swelling in the gums
Tooth discoloration (a sign of pulp death)
How Is Root Canal Treatment Performed?
Examination and X-ray: The extent and location of the infection are determined.
Anesthesia: The area is numbed to ensure a painless procedure.
Canal Cleaning: The infected pulp and tissues are removed, and the canals are disinfected.
Canal Filling: The cleaned and shaped canals are sealed with a special filling material.
Restoration: The tooth may be restored with a filling or crown to ensure durability.
With today’s advanced dental technologies, most root canal treatments can be completed in a single session.
Advantages of Root Canal Treatment
Preserves the natural tooth in the mouth
Maintains chewing function and aesthetic appearance
Prevents or delays the need for tooth extraction and prosthetics
Stops the spread of infection and bone loss
Has a success rate of over 95% when properly performed
Post-Treatment Care
Temporary sensitivity after treatment is normal
Avoid hard foods for the first 24 hours
Do not bite directly on the treated tooth until restoration is complete
Crowning may be recommended to strengthen the tooth
Maintain regular oral hygiene and dental check-ups
Frequently Asked Questions
Is root canal treatment painful?
No. The procedure is performed under local anesthesia, ensuring comfort. Mild soreness may follow but resolves quickly.
Can root canal treatment be done in one session?
Yes. Most simple cases are completed in a single visit. However, multiple sessions may be needed for advanced infections.
How long does a root canal-treated tooth last?
When properly done and maintained, such teeth can last 10–20 years or even a lifetime.
Will my tooth become fragile after treatment?
The tooth structure becomes slightly weaker, so a crown may be recommended to prevent fractures.
What if root canal treatment fails?
In such cases, the canal can be retreated (retreatment). For persistent cases, an apical resection (root-end surgery) may be required.
